ABA Billing Training for Professionals – Everything You Need to Know

Applied Behavior Analysis (ABA) billing is a specialized process that requires precision, compliance, and a deep understanding of insurance regulations. Professionals who master ABA billing training can streamline operations, reduce claim denials, and ensure seamless revenue cycles. This comprehensive guide will explore key components of ABA billing and common challenges, in addition to best practices and tips to optimize the billing workflow, including credentialing, contracting, and managing authorizations.
What Makes ABA Billing Unique?
ABA billing is distinct from other healthcare billing practices due to its specialized codes, compliance requirements, and multi-stakeholder involvement. Unlike general medical billing, ABA billing follows specific guidelines tailored to behavioral therapy services. Understanding these unique aspects is crucial for professionals handling claims, reimbursements, and working closely with insurance providers.
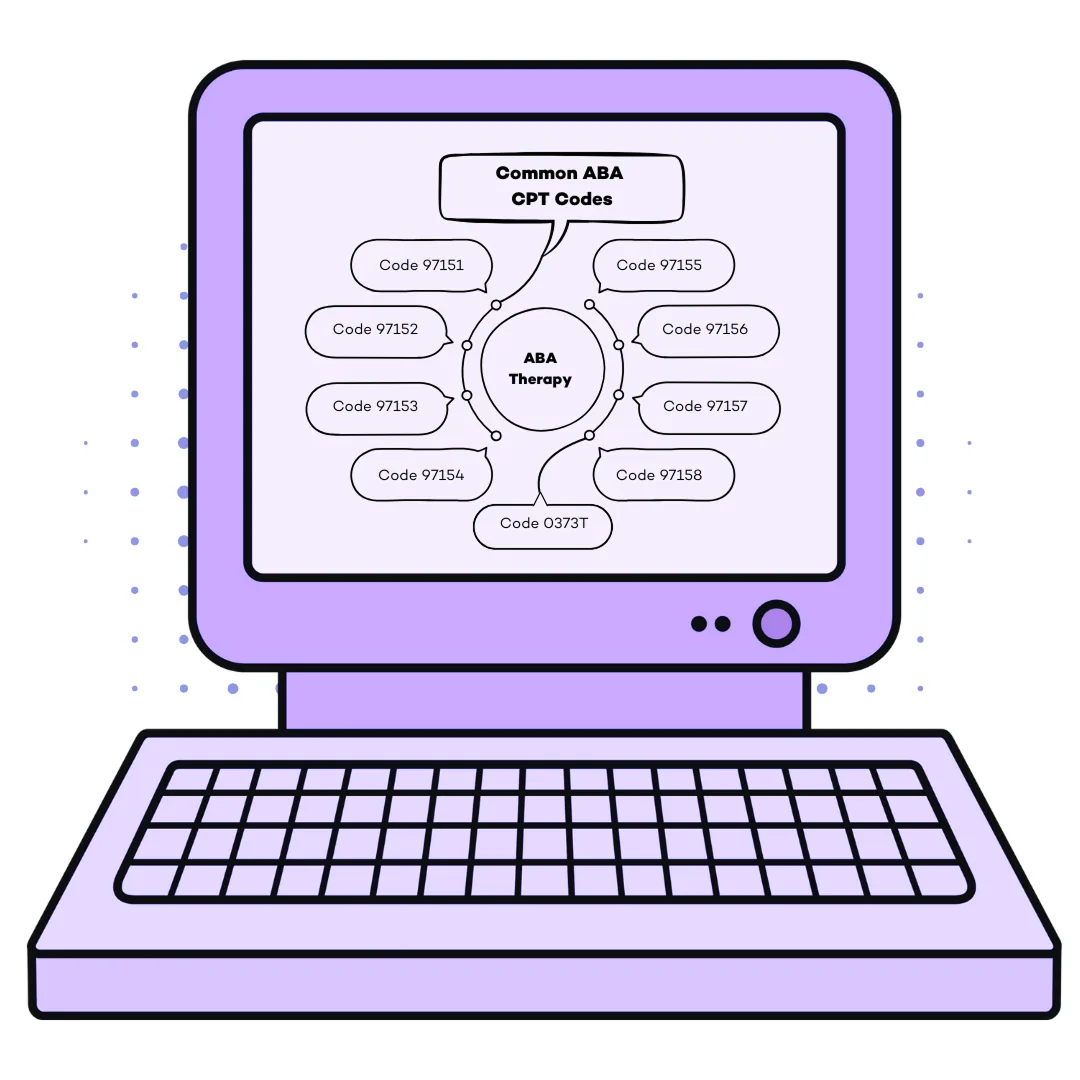
The Role of CPT Codes in ABA Billing
Stakeholders in ABA Billing
ABA billing involves multiple stakeholders, including insurance providers, therapists, and clients. Each party plays a critical role in ensuring that services are delivered, documented, and reimbursed correctly. Effective communication among stakeholders can prevent delays and streamline the billing process for ABA services. Behavioral therapists, including BCBAs and RBTs, must document services accurately, while billing professionals ensure claims are submitted according to insurance guidelines. Providers also rely on consulting services to navigate complex credentialing and contracting requirements. Parents or guardians may also be involved in verifying service logs and addressing billing inquiries. A coordinated effort among all stakeholders results in fewer billing errors and faster reimbursements.
Core Skills for Mastering ABA Billing
To excel in behavioral health billing, professionals must grasp essential training components. These elements provide the foundation for accurate and efficient billing practices, allowing learners to progress at their own pace while reducing claim denials and enhancing compliance.
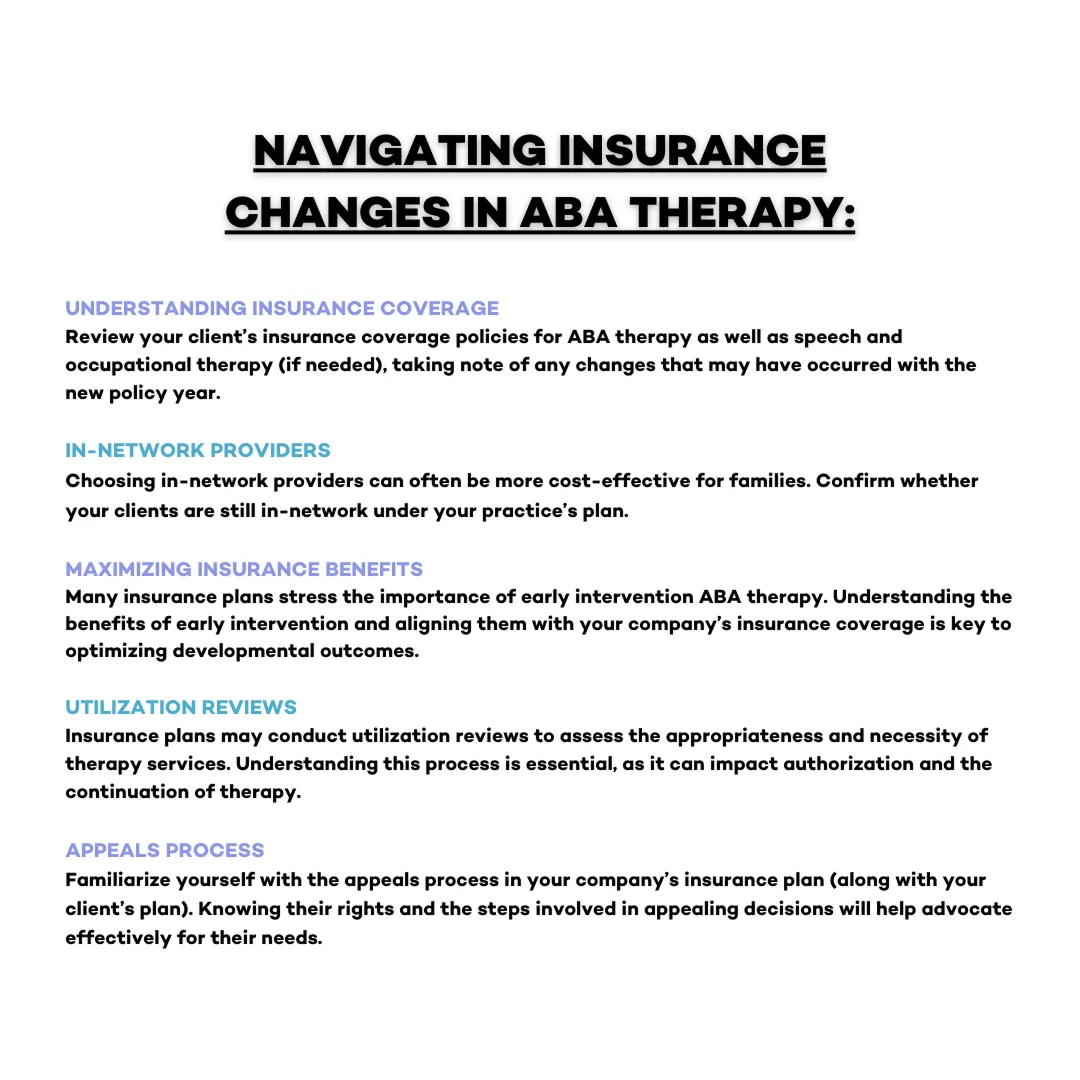
Understanding Insurance Billing Requirements
Mastering Claims Submission and Processing
Filing insurance claims correctly is critical to minimizing rejections and payment delays. Training in claim form completion, submission protocols, and follow-up procedures ensures smooth transactions between ABA therapy providers and insurance companies. Claim forms must be completed accurately with all required information, including service dates, CPT codes, and provider details. Errors in any of these fields can result in rejections or delays. A strong understanding of electronic payment processing systems, which expedite claim submission, is also essential for efficiency in modern billing practices. Additionally, managing authorizations effectively can prevent unnecessary denials and ensure claims are processed without delays.
Ensuring Compliance with HIPAA Regulations
Compliance with HIPAA and other healthcare regulations is mandatory for ABA billing professionals. Proper documentation, secure data handling, and adherence to regulatory guidelines protect client information and prevent legal issues. Professionals must be trained in secure data management, ensuring that sensitive client information remains confidential. Compliance training also covers fraud prevention, teaching professionals how to recognize and avoid billing practices that could lead to audits or penalties. Understanding federal and state-specific regulations is crucial for maintaining industry regulations across different regions. Some providers seek consulting services to ensure compliance with credentialing and certification requirements.
Common ABA Billing Challenges
Despite comprehensive training, professionals often face challenges—even with the basics of behavioral health billing. Identifying these pitfalls and implementing proactive solutions can enhance efficiency and increase revenue flow for ABA practices.
Preventing Claim Denials

Avoiding Common Pitfalls in ABA Billing
Billing errors, administrative inefficiencies, and miscommunication between stakeholders can create unnecessary business challenges. One of the most common pitfalls in ABA billing is the failure to obtain prior approvals, leading to claim rejections. Another frequent issue is improper documentation, which can result in audits or delays in reimbursement. Professionals must establish clear insurance billing protocols, maintain accurate business records, and consistently monitor regulatory changes to avoid these pitfalls.
Reducing Administrative Overload
Administrative inefficiencies, such as manual data entry and redundant processes, can burden ABA providers. Leveraging billing services and digital tools can streamline workflows, reduce errors, and enhance productivity. Many providers experience slow reimbursement due to inefficient processes, which can impact cash flow. Implementing automated billing solutions reduces time spent on repetitive administrative tasks and increases the accuracy of claims submissions. Additionally, outsourcing billing services to professionals with specialized knowledge can relieve in-house staff and improve overall business efficiency.
Streamlining Your Workflow with Efficient Systems
Optimizing the billing process involves integrating technology and structured workflows to enhance company efficiency. By adopting modern billing systems and best practices, professionals can improve accuracy and streamline operations.
How to Use Billing Software Effectively
Billing software solutions benefit ABA providers by managing claims, tracking reimbursements, and ensuring compliance with billing requirements. Choosing the right software and training staff to use it effectively enhances a company’s overall efficiency. Features such as automated claims tracking, real-time eligibility verification, and real-time reporting solutions can benefit providers in identifying potential billing issues before they escalate. Regular training sessions on software updates ensure that ABA therapy billing professionals stay up-to-date on their education and proficiency in utilizing all available tools to their complete potential.
Creating a Billing Workflow
Establishing a structured billing workflow improves consistency and compliance within a company. A well-defined workflow includes standardized procedures, automation software, and regular audits to maintain accuracy and reduce claim rejections. A streamlined billing workflow starts with verifying client eligibility and obtaining necessary clearances before services are rendered. The next steps include accurate records, proper coding, timely submission, and regularly scheduled follow-ups to address denied or pending claims. By implementing these structured workflows, ABA providers can significantly reduce insurance billing errors and start improving their overall revenue management.
Wrapping Up: Building a Strong Billing Foundation
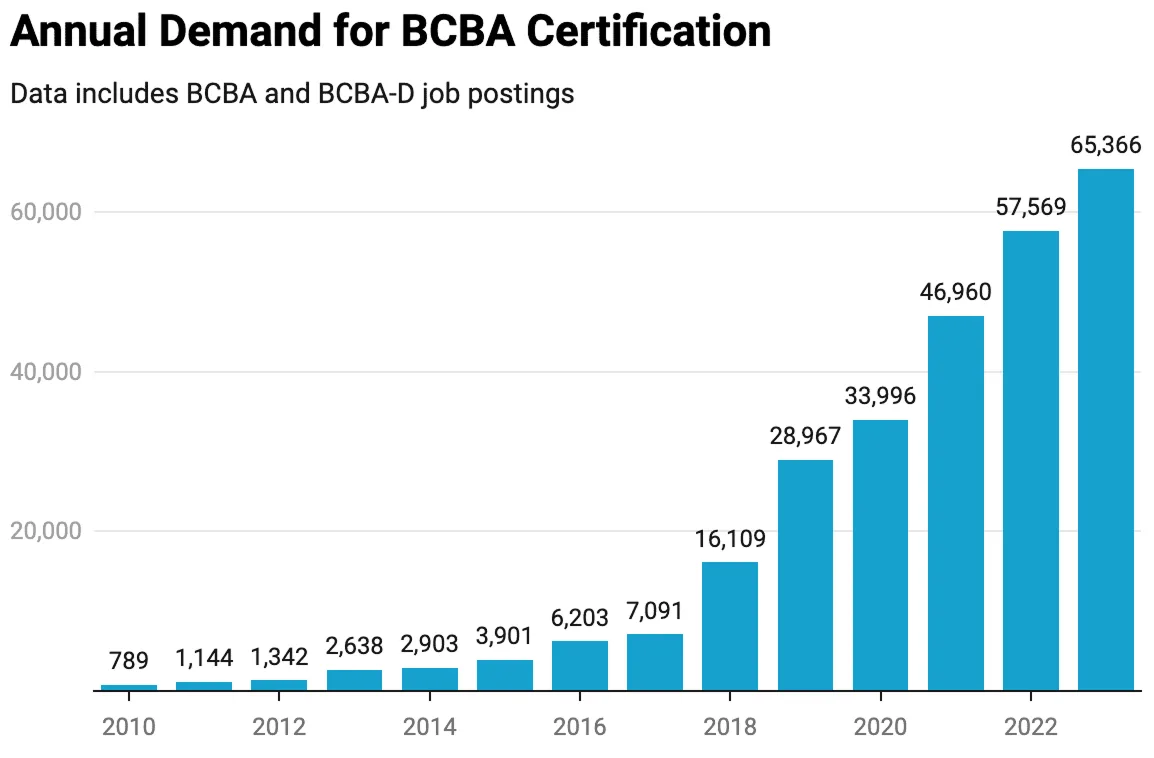
Mastering ABA therapy billing is essential for professionals looking to develop a complete, compliant, and efficient billing system. A well-structured approach ensures that ABA practices can meet the growing demand for high-quality behavioral therapy services while maintaining financial stability. By strengthening skills in insurance coverage requirements, claims processing, and workflow optimization, your ABA business can streamline operations and enhance revenue cycles.
Investing in comprehensive proper billing training helps your company stay ahead, reducing errors and maximizing reimbursements. A well-trained billing team allows providers to focus on delivering exceptional care to clients rather than dealing with administrative burdens.
For more tips and insights, explore our education resources on ABA billing training and discover ABA billing best practices. Additionally, learn more about ABA data collection and how to streamline your everyday billing with Raven Health’s integrated managed billing services.
When it comes to accuracy and efficiency, your team deserves the best so you can focus on what matters most: your clients.
Book a free 30-day trial today and get ready to experience seamless ABA billing firsthand.